The Newest Guideline To Basal Cell Carcinoma In 2023
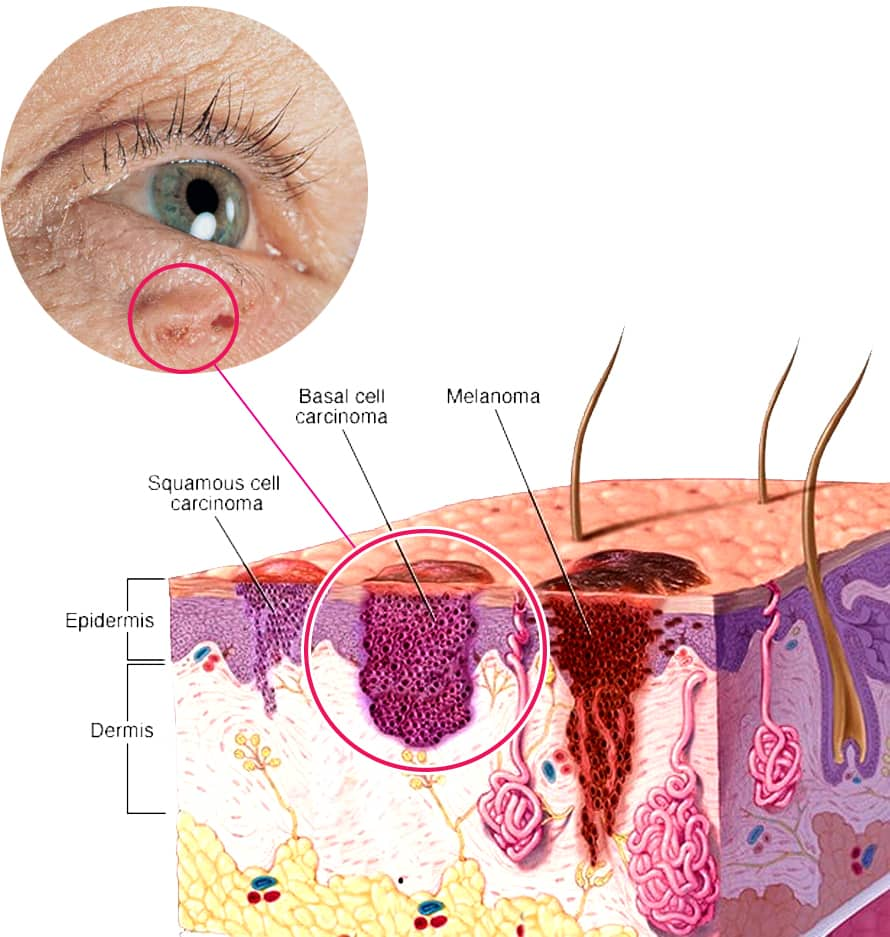
Basal cell carcinoma originates from basal cells. A type of cell inside the skin produces new and fresh skin cells when the old cells are destroyed.
Basal cell carcinoma often appears as a slightly clear bump on the skin, although it can also appear in other forms.
What causes basal cell carcinoma?
Basal cell carcinoma is a type of skin cancer. Basal cell carcinoma originates from basal cells. A type of cell in the skin produces new skin cells as old cells die.
Basal cell carcinoma occurs more often in areas of the skin exposed to the sun, such as the head and neck.
Most DNA damage in basal cells appears to result from ultraviolet (UV) radiation from sunlight and tanning beds. However, exposure to the sun causes skin cancers that occur on the skin, generally exposed to sunlight. Also, other factors can play a role in basal cell cancer risk and occurrence; in some cases, the exact cause may not be clear.
Most basal cell carcinomas are thought to be caused by long-term exposure to ultraviolet (UV) radiation from sunlight. Avoiding the sun and using sunscreen may help protect against basal cell carcinoma.
What are the symptoms of basal cell carcinoma?
Basal cell carcinomas develop in body parts usually exposed to the sun, especially the head and neck. Sometimes, basal cell carcinoma can also develop in body parts not generally protected from the sun, such as the genitals and perineal.
Basal cell carcinoma appears as changes in the skin, such as growths or sores and nodular or exophytic that do not heal.
These changes in the skin (damages) usually have one of the following characteristics:
- Pearly white, skin-colored, or pink bumps are usually straightforward, meaning you can see a small quantity on the skin’s surface. They may also be visible as tiny blood vessels. The lesion may be darker but still somewhat transparent in people with dark skin. The lesion is the most common type of basal cell carcinoma that often appears on the face and ears. Also, this lesion may tear, bleed, and crust
- A brown, black, or blue lesion or a lesion with dark spots and a slightly raised and clear border.
- A patch of extra, smooth, scaly, reddish skin with a raised edge, mostly seen on the back or chest. Also, over time, these patches can become very large.
- A white, waxy, ulcer-like lesion with no clear border, called basal cell carcinoma, is usually less common.
When should you see a doctor?
See your doctor if you notice changes in the appearance of your skin, such as new skin growth, changes in previous growth, or frequent sores.



How is basal cell carcinoma diagnosed?
In order to evaluate any growth or change in the skin, a doctor or dermatologist (dermatologist) will perform a history and medical examination. In other cancers, cancer screening is used.
- History and general conditions of the patient: The doctor will do a general physical exam and ask about your medical history, skin changes, or any other signs or symptoms you have been experiencing.
- Skin examination: The doctor examines not only the suspicious area on the skin but also other parts of the body for other lesions.
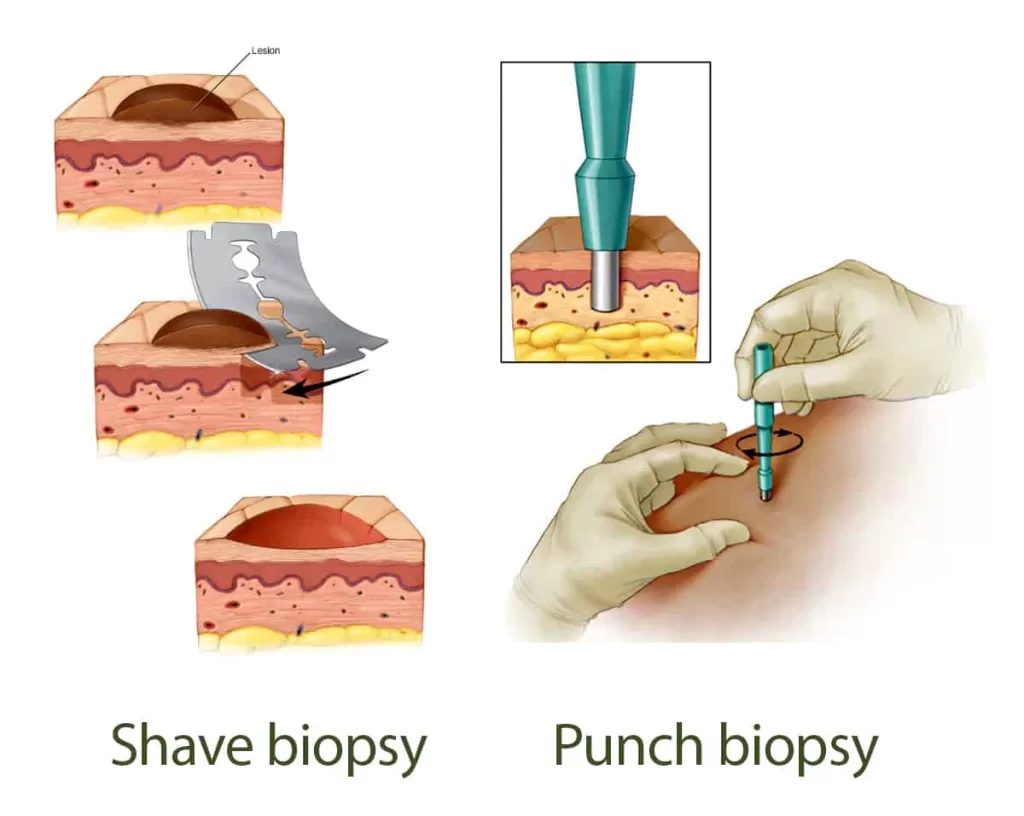
- Taking a sample from the skin for testing: A doctor may perform a skin biopsy, which involves removing a small lesion sample for testing in a laboratory. This procedure is done to determine if you have skin cancer or not and, if so, what type of skin cancer you have. The type of skin sampling depends on the type and size of the lesion.
reference : “https://www.mayoclinic.org/“
Factors that increase the risk of basal cell cancer include:
Exposure to intense sun. Spending much time under the sun or in a solarium increases the risk of basal cell cancer. If you live in a sunny place or at a high altitude, you are more exposed to UV rays. Severe sunburn can also increase the risk.
- Radiotherapy. Radiation therapy to treat acne or other skin conditions may increase the risk of basal cell carcinoma in previously treated skin areas.
- Light skin. The risk of basal cell carcinoma is higher among people who have freckles or burn quickly or have very fair skin, red or blond hair, or light-colored eyes.
- Age increasing. Because basal cell carcinoma often takes decades to develop, most basal cell carcinomas occur in older adults. However, it can also affect young adults and is more common in people in their 20s and 30s.
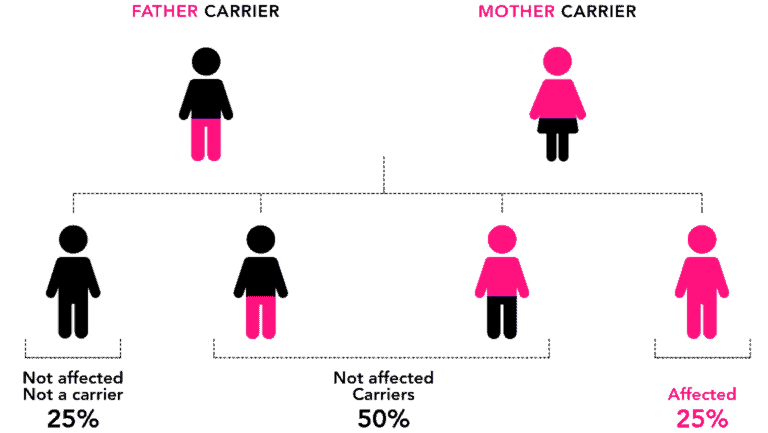
- Personal or family history of skin cancer. If you have been diagnosed with basal cell carcinoma once or more, the chances of it developing again are very high. Your risk of developing basal cell carcinoma may increase if you have a family history of skin cancer.
- Immunosuppressive drugs. Taking drugs that suppress the immune system, such as anti-transplant rejection, significantly increases skin cancer risk.
- Arsenic exposure. Arsenic, a toxic metal widely found in the environment, increases the risk of basal cell carcinoma and other cancers. Naturally, everyone is exposed to arsenic to some extent. However, some people may be more exposed to arsenic if they drink contaminated well water or have a job involving arsenic production or use.
- Hereditary syndromes that cause skin cancer. Some rare genetic diseases, including nevoid basal cell carcinoma syndrome (Gourlin-Goltz syndrome) and xeroderma pigmentosum, can increase the risk of basal cell carcinoma.
Can basal cell carcinoma be prevented?
To reduce the risk of basal cell cancer, you can:
- Avoid being in the sun in the middle of the day. The sun’s rays are most potent in many places between 10 am and 4 pm. Postpone outdoor activities to other times of the day, even in winter or when the sky is cloudy.
- Use sunscreen all year round. Even on cloudy days, use a broad-spectrum sunscreen with an SPF of at least 30. Apply sunscreen continuously and reapply every two hours if you swim or sweat more.
- Wear protective clothing. Cover your skin with dark, tightly woven clothing that covers the arms and legs and a wide-brimmed hat, which provides more protection than a baseball cap or protective cloth.
- Remember the sunglasses. Look for glasses that control both ultraviolet rays (UVA and UVB).
- Do not use the solarium. Tanning beds emit UV rays and can increase the risk of skin cancer.
- Check your skin regularly and report any changes to your doctor. Check your skin often for new growth or changes in moles, freckles, bumps, and birthmarks. Check your face, neck, ears and scalp with the help of a mirror.
- Examine the chest, upper body, and upper and lower parts of the arms and hands. Check the front and back of the legs and the bottom of the legs, including the soles and the distance between the toes. Also, check the genital area and between the buttocks.
Can basal cell carcinoma be cured?
The goal of basal cell cancer treatment is to obliterate cancer. Which treatment method is best depends on the type, location, and size of the cancer, your preferences and your ability to make follow-up visits. Treatment choice can also depend on whether it is a first-time, Non-Invasive, or recurrent basal cell carcinoma.

What are the treatment options for basal cell carcinoma?
Basal cell carcinoma is often treated with surgery to remove all of the cancer and some of the surrounding healthy tissue. If basal cell carcinoma is at high risk of recurrence, surgery may be recommended, for example, if it is more significant or more profound in the skin. Expanded or placed in the face.
Other treatment methods may be recommended in certain situations, such as when you cannot or do not want surgery.
Other treatments include:
- Curtage and electrodissection (C and E). C and E treatment involves removing the surface of the skin cancer with a scraping tool (curt) and then burning the cancerous tissue with an electric needle.
- Radiotherapy. In radiation therapy, high-energy rays such as X-rays and protons are used to destroy cancer cells. Radiation therapy is sometimes used after surgery when the cancer is more likely to return. It may also be used in the absence of surgery.
- Cryotherapy. This treatment involves freezing cancer cells with liquid nitrogen (cryotherapy). This may be an option for treating superficial skin lesions. Freezing may be done after using a scraping tool (curt) to remove the surface of the skin cancer.
- In the absence of surgery, cryotherapy may be considered to treat minor and thin basal cell carcinoma.
- Topical treatments. A prescription cream or ointment may be considered to treat minor and thin basal cell carcinoma without surgery.
- Photodynamic therapy. Photodynamic therapy is a combination of light-sensitive drugs to treat superficial skin cancers. During photodynamic therapy, liquid medicine that sensitizes cancer cells to light is placed on the skin. Later, a light that destroys the skin cancer cells is shined on the area.
- In the absence of surgery, photodynamic therapy may be considered. Treatment with chemotherapy is less common.
Rarely, basal cell carcinoma may spread (metastasize) to nearby lymph nodes and other body areas. Additional treatment options for this condition include:
Targeted drug therapy. Targeted drug therapies focus on specific weaknesses in cancer cells. By blocking these vulnerabilities, targeted drug therapies can kill cancer cells.
Targeted therapies for basal cell carcinoma block the molecular signals that enable cancers to grow. They may be considered after other treatments or if other treatments are impossible.
Chemotherapy. In chemotherapy, powerful drugs are used to destroy cancer cells. If other treatments have not helped, this method may be a treatment option.
Conclusion
Basal cell carcinoma (BCC) is the most common form of skin cancer among white people.
BCC is usually not life-threatening, but if left untreated, it can cause significant disfigurement, especially of the face.
Surgery to remove the affected area and surrounding skin is usually the first option for BCC treatment. There are several different surgical procedures and non-surgical treatments, such as radiation therapy (high doses of radiation that kill cancer cells) and anti-cancer creams, gels, and ointments.
Share in :
Explore more


Collagen Benefits For Hair And Skin- Drhealthandbeauty