
What Are The Risks Of A Pancreas Transplant?
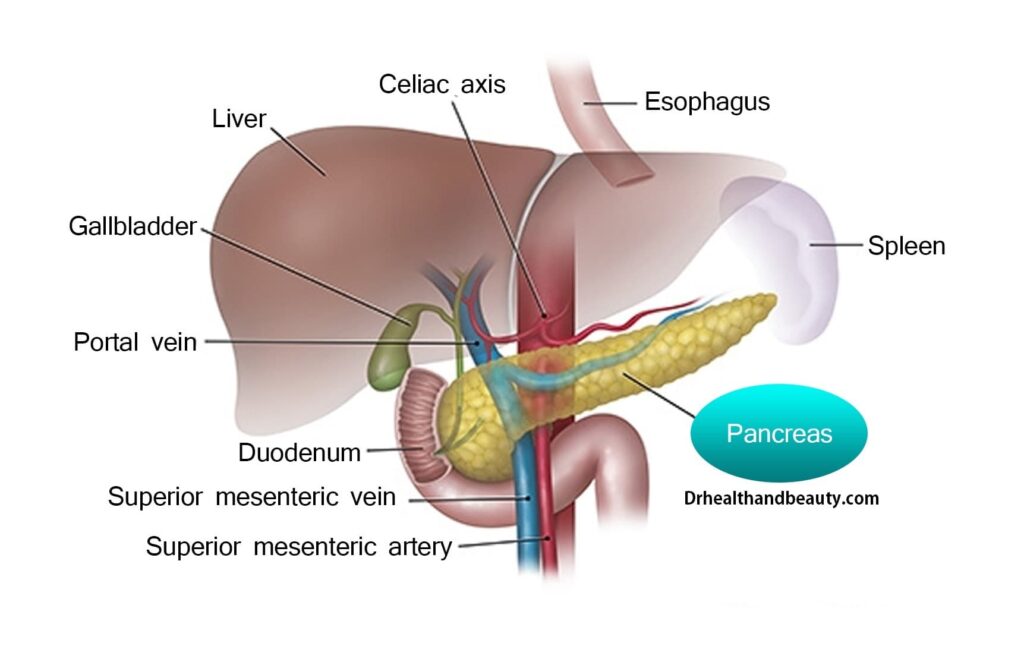
A pancreas transplant is a surgery that combines a healthy pancreas from a deceased donor with a pancreas from someone who is not working well. Pancreas is an organ in the lower abdomen whose primary function is insulin as a hormone for the absorption of sugar by cells. If your pancreas does not produce enough insulin, unhealthily high blood sugar can lead to type 1 diabetes.
A Pancreas transplant is one of the chosen options for treating diabetes, which, like other surgeries, has complications and is a significant operation. Some Pancreas Transplant complications may occur soon after the operation, while others may occur months or years later. Some of the main risks associated with a pancreas transplant are described below.
A pancreas transplant can cure diabetes and eliminate the need for insulin injections. However, this method is not standard due to the risks of surgery. This article by Drhealthandbeauty describes the risk of a pancreas transplant.
Table of Contents
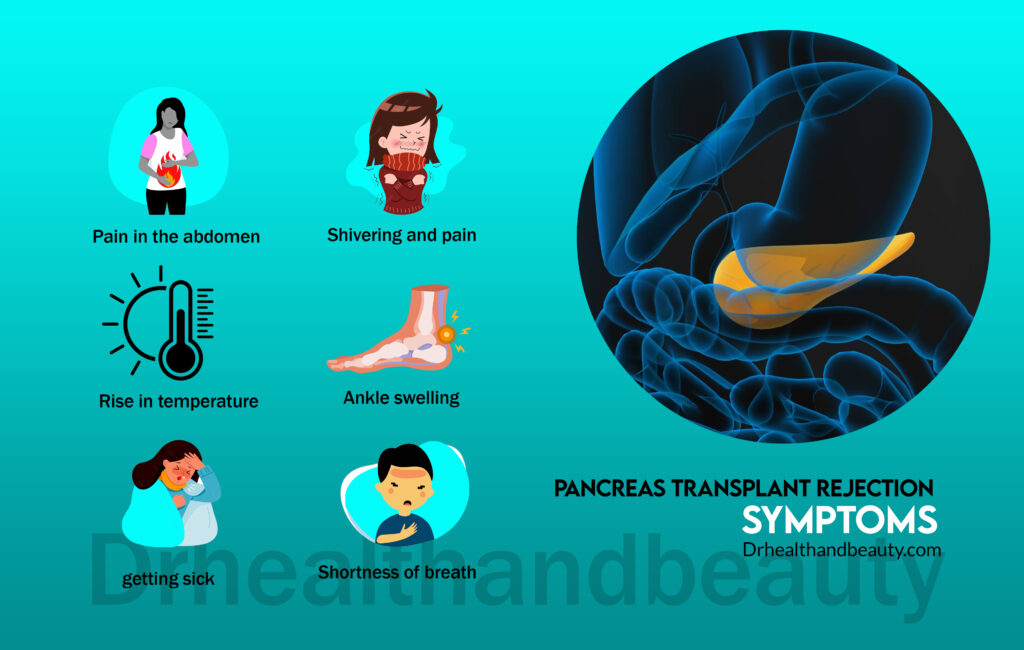
Rejection of Pancreas Transplant
One of the most common complications of pancreas transplantation is the rejection of the donor pancreas. This is where the immune system recognizes the transplanted pancreas as foreign and attacks it.
Rejection of the pancreas usually occurs within days, weeks, or months after the transplant, although it can sometimes occur years later. Immunosuppressive drugs can reduce the risk of transplant rejection.
Pancreas Transplant rejection symptoms are:
- Pain and swelling in the abdomen
- rise in temperature
- getting sick
- Shivering and pain
- severe fatigue
- ankle swelling
- Shortness of breath
If you have these symptoms, contact your doctor as soon as possible. Pancreas Transplant rejection is usually treated by increasing the dose of immunosuppressive drugs.
Immune system suppressive side effects
The immunosuppressive drugs that you must take to prevent rejection may have significant side effects, including:
- Increased risk of infection
- Shaking hands
- Difficulty sleeping
- Increased blood pressure
- hair loss
- Mood swings
- Weight Gain
- stomach ache
- Rash and redness of the skin
- weakened bones (osteoporosis)
- Increased risk of certain types of cancer, especially skin cancer
Talk to your transplant team if you experience any side effects. Do not stop taking medications without consulting your doctor.
Infections after Pancreas Transplant
Immunosuppressive drugs weaken the immune system and increase the chance of infection.
Keep the following things in mind while taking Pancreas Transplant medicine:
- Report possible symptoms of infection to your doctor right away – these include fever, muscle pain, diarrhea, or headache.
- Make sure your vaccinations are up-to-date – talk to your GP for advice on which additional vaccines are needed, as some carry a risk of illness if you take immunosuppressants.
- Avoid close contact with anyone who has an infection—even if it is an infection like chickenpox that you are already immune to.
- To help prevent infection, you may be given antibiotics, antifungal medications, or antiviral medications for the first few weeks or months after your transplant.
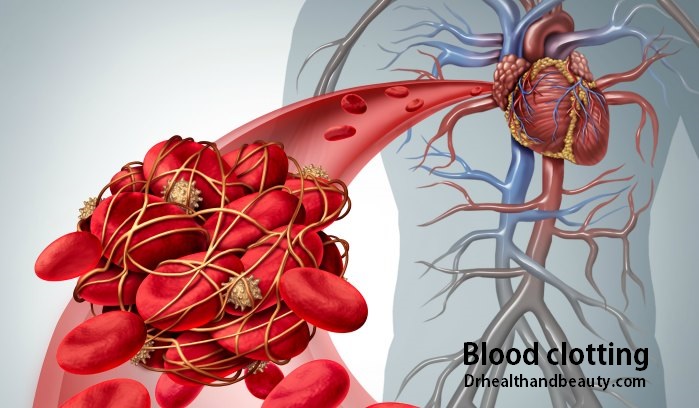
blood clotting
Sometimes blood clots form in the blood vessels supplying the new pancreas, preventing it from working correctly.
The risk of this happening is more significant in the days following the operation so that you will be closely monitored in the hospital for any signs of a blood clot. You will also be given a blood thinner to reduce the chance of clot formation.
If a blood clot forms in the new pancreas, you usually need another surgery to remove it.
After Pancreas Transplant surgery, blood clots can form in other blood vessels, such as the legs (deep vein thrombosis) or the arteries supplying the lungs (pulmonary embolism). However, the use of blood thinners can prevent them. This will help.
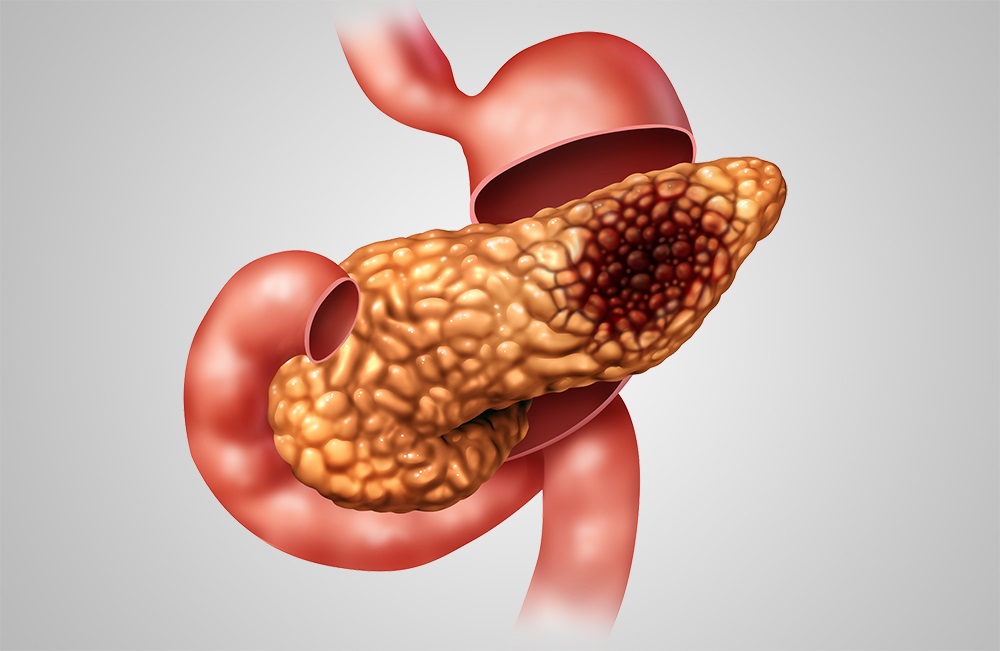
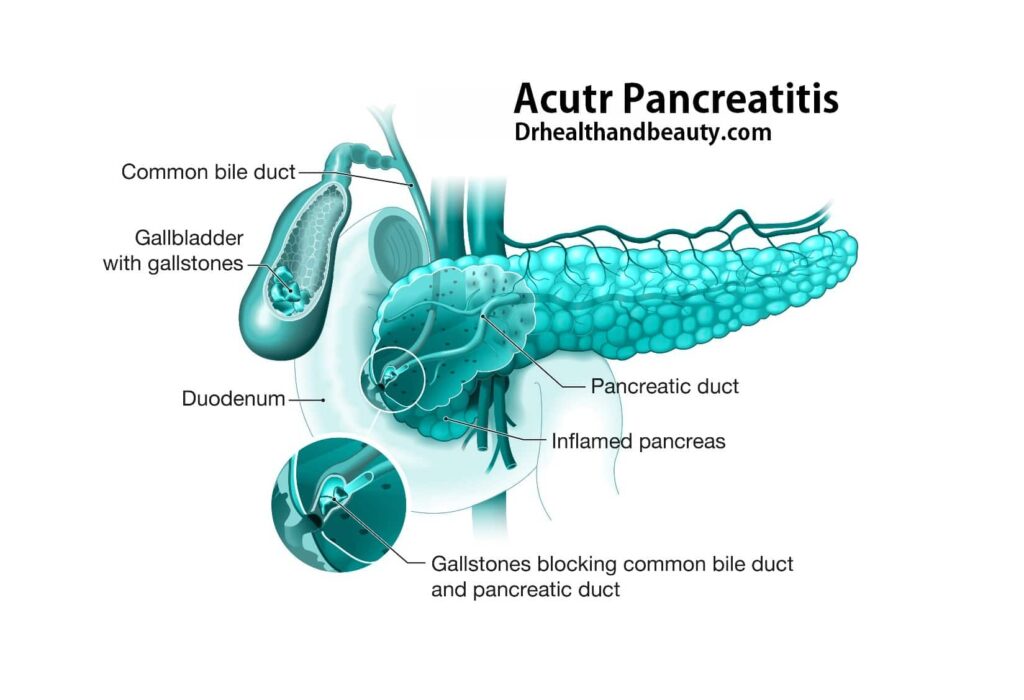
inflammation of the pancreas (pancreatitis)
Pancreatitis is swelling and inflammation of the pancreas and is expected in the first few days after surgery. This can happen because the donor’s pancreas is stored on ice in preparation for the transplant.
Symptoms of pancreatitis include the following:
- Dull pain in the abdomen
- Feel sick
- Vomit
Pancreatitis should resolve within a few days. However, sometimes tubes may be placed in your abdomen to drain excess fluid from the donor pancreas, and in a few cases, it may need to be removed.
Pancreas transplants can cause the production and accumulation of insulin again in people with diabetes. However, this is not a standard treatment. The side effects of the drugs used to prevent rejection of the Pancreas Transplant can be severe.
After Pancreas Transplant:
You will stay in the intensive care unit for a few days: doctors and nurses constantly evaluate your condition. The new pancreas starts working immediately, and the old pancreas continues its other functions.
If you have a new kidney, it will produce urine, just like your own kidney. Most of the time, the new kidney starts working quickly, but sometimes it may take a few weeks to reach the average level of urine production.
You will stay in the hospital for about a week: after the condition stabilizes, you will be transferred to the recovery ward. At this stage, you may feel some pain or burning at the incision site until you fully recover.
You will have frequent examinations to continue your recovery: after leaving the hospital, it is necessary to evaluate your condition for 3 to 4 weeks. So if you live in another city, it is better to take measures to be close to the transplant center at this time.
You will need to take medication for the rest of your life: After a pancreas transplant, you will receive several medications to suppress your immune system, preventing your body from starting an immune response to the new pancreas.
Other medications may also be used for problems such as high blood pressure or infections.

Life after pancreas transplant surgery
After the pancreas transplant, anti-rejection drugs are prescribed to prevent the transplant organ’s rejection by the individual’s immune system.
A person considered for a transplant must be willing to take anti-rejection drugs for the rest of their life. In addition, he must be willing to undergo lifelong follow-up tests by health care professionals.

Pancreatic transplant drugs
The risks of this procedure are infection and organ rejection. Rejection occurs when the body’s immune system attacks the new organ as a new “foreign” invader. To reduce the chances of rejection, the healthcare team tries to match the donor’s blood and tissue type with the transplant recipient.
After the transplant, doctors prescribe certain drugs, such as azathioprine and cyclosporine, to suppress the immune system to prevent rejection of the new pancreas. However, these drugs increase transplant recipients’ risk of infections such as colds and flu.
Over time, these drugs may also increase the risk of certain cancers. For example, it is essential to cover the skin and use sunscreen because of the increased risk of skin cancer. If you have a pancreas transplant, you must take certain medications as long as you have the organ in your body.
You will also need to have tests over the years to ensure your pancreas transplant is still working correctly. It is also essential to keep all of your doctor’s appointments.

Conclusion
A pancreas transplant is a surgery in which you receive a healthy donor pancreas.
A Pancreas transplant is the most appropriate option for some people with type 1 diabetes. Type 1 diabetes is an autoimmune disease in which the pancreas stops producing the hormone insulin. The usual treatment for type 1 diabetes involves daily insulin injections.
You will receive a healthy pancreas from a deceased donor during a pancreas transplant. If your diabetes has caused kidney failure, your surgeon may also perform a kidney transplant at the same time. Kidney transplants can be done before or even after a pancreas transplant.
In a pancreas transplant, your pancreas stays in your body. The surgeon generally attaches the new pancreas to your intestine so that it may leak digestive juices. After a successful transplant, you will no longer need to take insulin. Instead, the new pancreas will ask for insulin for you. You can also have a regular diet. You will have few or no episodes of low (or very high) blood sugar or insulin shock, and your chances of kidney damage will be reduced.
Share in :
Explore more


Sitting A Long Time And Being Overweight- Drhealthandbeauty

