
What are colitis ulcerative symptoms?
Intestinal colitis or Colitis ulcerosa is an inflammatory bowel disease (IBD) that causes long-term inflammation and ulcers in the digestive tract.
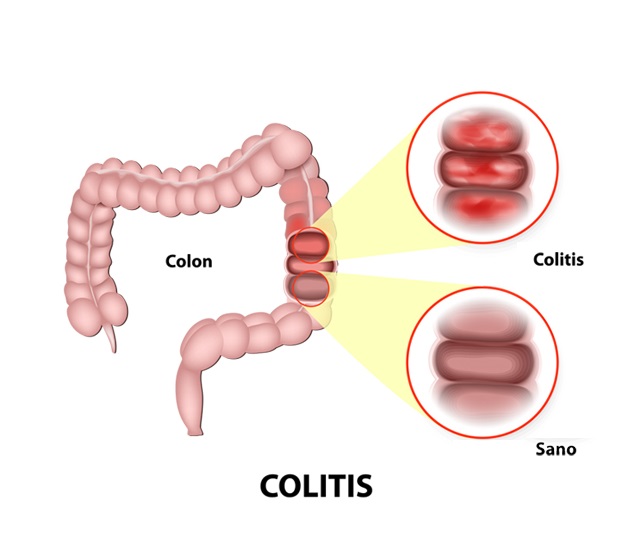
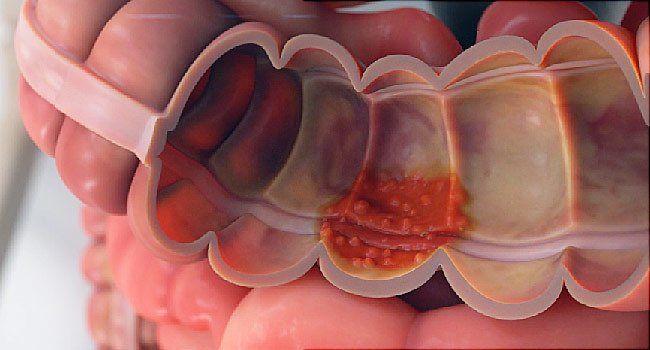
ulcerosa colitis belongs to a group of diseases called inflammatory bowel disease (IBD). IBD, or inflammatory bowel disease, includes a group of diseases that affect the digestive system. The inflammation starts from the rectum and gradually involves the colon. There is no healthy zone between the involved sectors. ulcerosa Colitis occurs when the lining of the large intestine, the rectum, or both become inflamed. Usually, colitis involves the innermost layer and causes inflammation. This inflammation causes small ulcers in the large intestine.
Intestinal inflammation causes bowel contents to be excreted more quickly, and the bowel is emptied more frequently. Ulcers form as cells on the surface of the intestinal lining die. Ulcers may bleed and ooze mucus.
Table of Contents
ulcerosa colitis is a chronic disease that can be controlled with treatment, but no definitive cure exists. This means that the disease has a long course but is not fatal. Treatment can reduce the signs and symptoms of the disease and even cause long-term recovery. Most people with ulcerative colitis lead an everyday and valuable life. People of different ages can get this disease; most people with this disease are between 15 and 35 years old.
Signs and symptoms of colitis
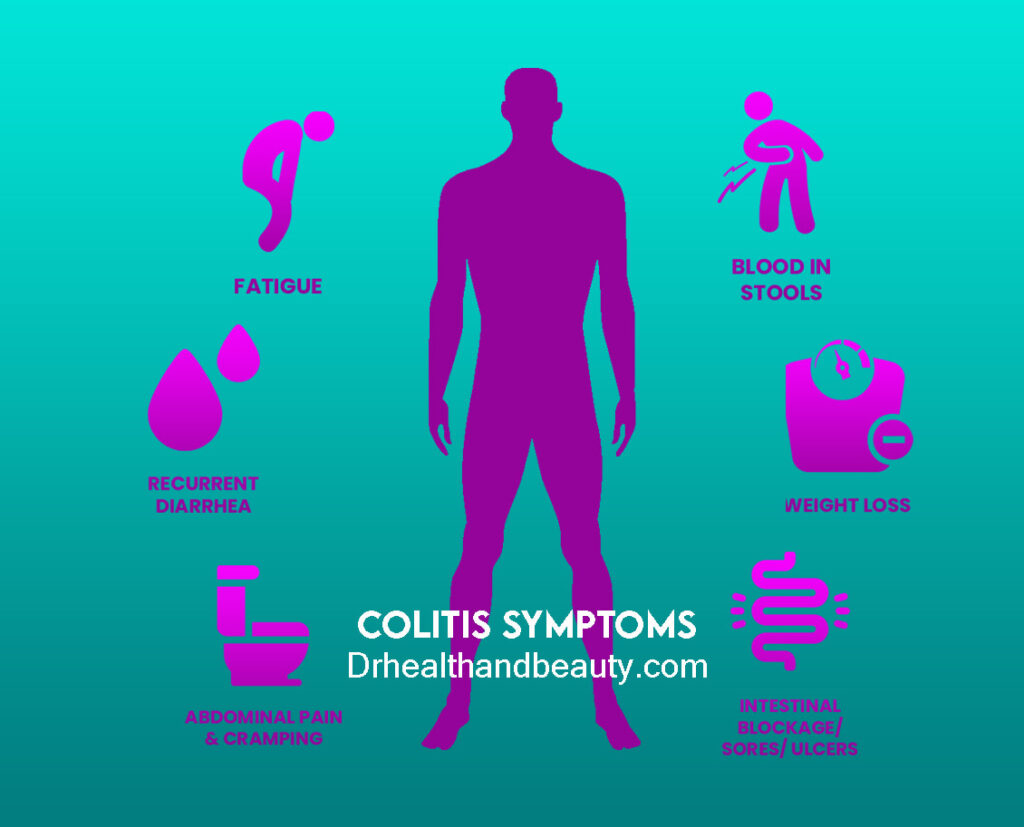
ulcerosa Colitis symptoms depend on the severity of the inflammation and the location of the inflammation. Signs and symptoms of Ulcerative Colitis include:
Diarrhea, often with blood
Abdominal pain and intestinal cramps
rectal pain
Rectal bleeding – passing a small amount of blood into the stool
The urgent urge to defecate
Weight Loss
tiredness
Failure to thrive in children
Most people with ulcerosa colitis have mild to moderate symptoms. The course of colitis may vary; some people have longer courses.
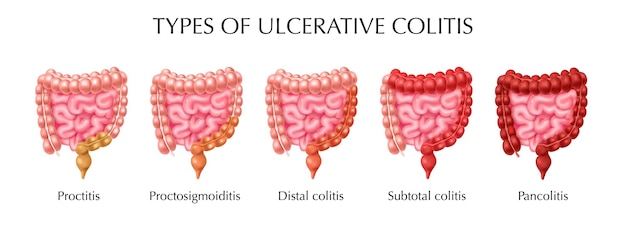
Types of ulcerative colitis
Doctors often classify ulcerative colitis according to where it occurs. The types of ulcerative colitis are:
Ulcerative proctitis refers to inflammation limited to the rectal area; this type of rectal bleeding occurs intermittently. This form of colitis is milder.
Proctozygomitis inflammation includes the rectum and sigmoid colon (a short part of the place where the large intestine joins the anus). Signs and symptoms include bloody diarrhea, abdominal cramps and pain, and the inability to move the bowels despite the desire to do so (tenesmus).
Left-sided colitis includes inflammation from the rectum to the sigmoid and the descending part of the large intestine. Signs and symptoms include bloody diarrhea, abdominal cramping, left-sided abdominal pain, and unwanted weight loss.
Pancolitis or total colitis refers to swelling and inflammation of the entire large intestine (right colon, left colon, transverse colon, and anus). Pancolitis often causes bloody diarrhea, which may be severe. Other symptoms include abdominal cramping and abdominal pain, fatigue, and significant weight loss.
Ulcerative or malignant colitis is a rare but severe form of pancolitis. This rare colitis affects the entire colon and causes severe pain, profuse diarrhea, bleeding, fever, and inability to eat.
Causes and causes of ulcerative colitis
A variety of diseases and infections can cause the cause of colitis and colon inflammation. Some of the most common causes and possible factors of colitis are:
- Infectious colitis
Viruses and bacteria can cause colon infections and cause ulcerative colitis. Most of them cause foodborne illnesses or food poisoning. The most common bacteria that cause infection are Shigella, Ecoli, Salmonella, and Campylobacter. These infections may also cause bloody diarrhea.

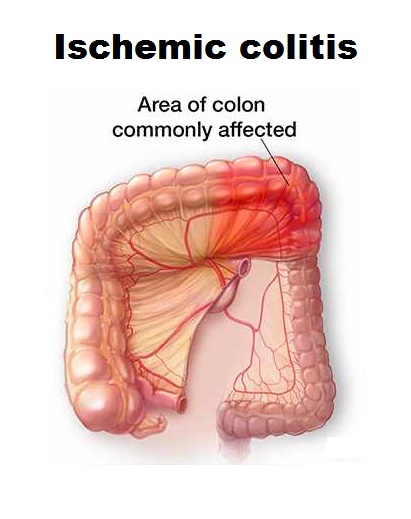
- Ischemic colitis
One cause of colitis is decreased blood supply to the large intestine. The arteries that supply blood to the intestines are like any other arteries. Arteries can become narrowed due to atherosclerosis (like blood vessels in the heart that can cause angina or narrowed vessels in the brain that can cause a stroke). When these arteries are narrowed, the blood supply to the colon may be disturbed, and the colon may become inflamed.
The colon can also lose blood mechanically. These include mechanical torsion, where the bowel wraps around itself, or an obstructive hernia, where part of the colon is trapped in the abdominal wall, blocking blood flow to the affected area. Ischemia, or lack of proper blood supply, causes pain, fever, and bloody bowel movements.
- Inflammatory bowel disease (IBD) and ulcerative colitis
There are two types of inflammatory bowel disease:
- ulcerative colitis
- Crohn’s disease.
Colitis is thought to be caused by an autoimmune disease in which the body’s immune system attacks the colon and causes inflammation. Ulcerative colitis begins in the rectum and may gradually spread throughout the colon. Signs and symptoms include abdominal pain and bloody bowel movements.
Crohn’s disease may cause inflammation in any part of the digestive system, from the mouth, esophagus, and stomach. Crohn’s often has infill lesions, meaning that the affected areas overlap with areas of healthy tissue.
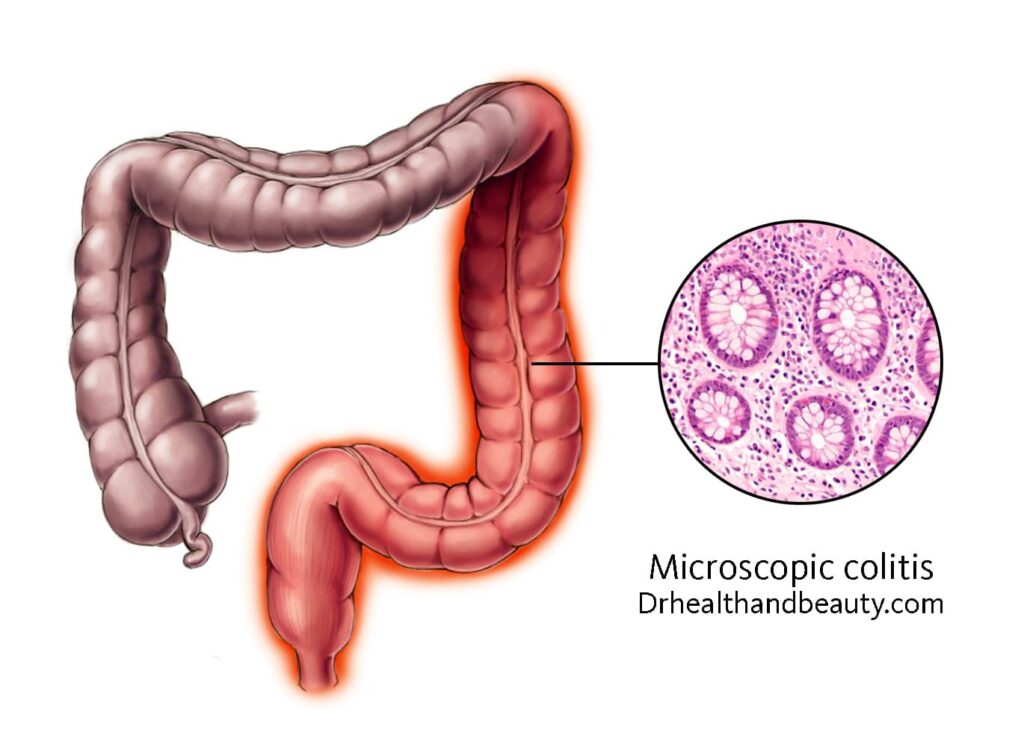
- Microscopic colitis
In this type of colitis, there are two types of inflammation: collagen colitis and lymphocytic colitis of the colon; the cause of colitis in these cases is due to the inflammation caused by collagen and lymphocytes. Watery diarrhea is the most common symptom of this type of colitis. This is an uncommon disease that is more common in older women. The cause of microscopic colitis is still unknown, but the autoimmune potential may exist.
- Molecular colitis
The cause of molecular colitis is the injection of foreign substances into the large intestine. If chemicals are injected into the colon, inflammation, and damage can occur. One of its complications is mucosal inflammation caused by external chemicals.
- Drug-related ulcerosa colitis
Colitis can be caused by some contraceptive and prescription drugs such as nonsteroidal anti-inflammatory drugs (NSAIDs), mycophenolate, ipalimibob, and retinoic acid.
People at risk of ulcerative colitis
Ulcerative colitis can affect both men and women. The risk factors of ulcerative colitis are:
Age. Ulcerosa colitis usually begins before age 30, But it can occur at any age, and some people may not have the disease until age 60.
Race or Ethnicity Although whites have the highest risk of developing the disease, ulcerative colitis can occur in any race. Jews have a higher risk of developing ulcerative colitis.
Family history. You are at increased risk if you have someone close to you, such as a parent, sibling, or sibling, with ulcerative colitis.
Complications of ulcerative colitis
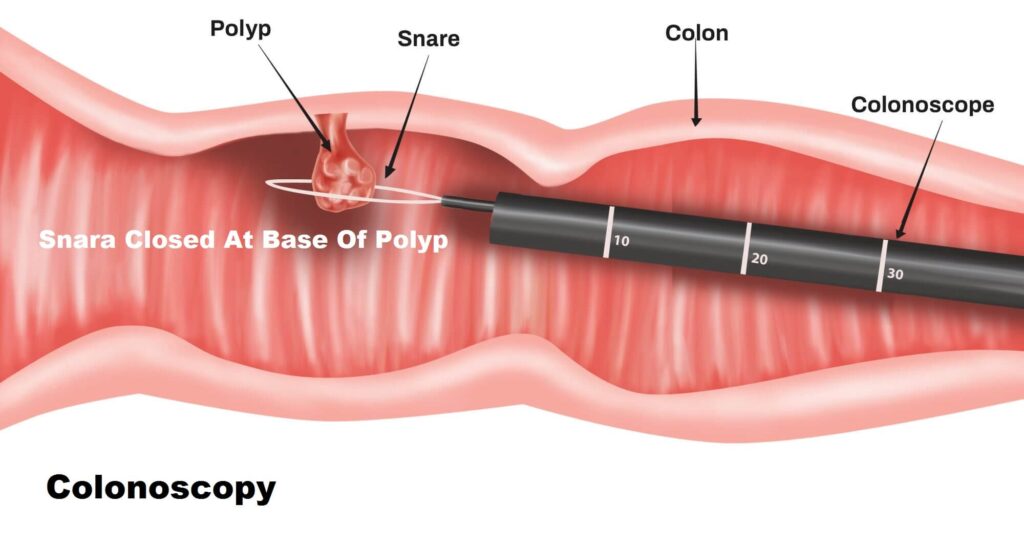
Ulcerative colitis increases the risk of colon cancer. Because of this increased risk, your doctor will perform a colonoscopy and check for cancer when diagnosed with colitis. Regular screening helps reduce the risk of colon cancer. With follow-up, it can detect pre-cancerous cells early.
Other complications of ulcerative colitis include:
The thickness of the intestinal wall
Sepsis, or blood infection
Severe dehydration
liver disease (rare)
Intestinal bleeding
kidney stone
Inflammation of the skin, joints, and eyes
Rupture of the colon
Ankylosing spondylitis, or inflammation of the joints between the bones of the spine

Treatment of gastric colitis
Ulcerative colitis treatment usually includes drug therapy or surgery. Several classes of medications may be effective in treating ulcerative colitis. The type of medicine prescribed for the patient depends on the severity of his disease; the medicines that work well for some people may not be effective for others. In addition, since some medications have serious side effects, the benefits and risks of each treatment must be weighed.
- Anti-inflammatory drugs
Anti-inflammatory medications are often the first step in treating ulcerative colitis and are appropriate for most people with the disease. These drugs include:
- Amino salicylates
Examples of this type of drug are sulfasalazine (Azulfidine), mesalamine (Delzicol, Rovasa), balsalazide (Colazal), and olsalazine (Dipentum). The type of medicine and how to take it (oral, enema, or suppository) depends on the part of the large intestine affected by the disease. These drugs must be taken with the doctor’s opinion, otherwise, do not take these drugs at all.

- Corticosteroids
These drugs, which include prednisone and budesonide, are usually prescribed for moderate to severe ulcerative colitis that has not responded to other treatments. Corticosteroids suppress the immune system. Because of side effects, they are usually not prescribed long-term. These drugs must be taken with the doctor’s opinion, otherwise, do not take these drugs at all.
- Immunosuppressive drugs include:
Azathioprine (Azasan, Imuran) and mercaptopurine (Purinethol, Purixan): These immunosuppressants commonly treat inflammatory bowel disease. Immunosuppressive drugs require careful follow-up by a doctor and regular blood tests to check for side effects, including effects on the liver and pancreas.
Cyclosporine (Gengraf, Neoral, Sandimmune): This drug is usually prescribed for people who have not responded well to other drugs. Cyclosporine has many side effects and is not recommended for long-term use.
- Biological drugs
These drugs target proteins made by the immune system. The types of biological drugs used in the treatment of ulcerative colitis are:
Infliximab (Remicade), adalimumab (Humira), and golimumab (Simponi): These are called tumor necrosis factor (TNF) inhibitors. These drugs work by neutralizing proteins produced by the immune system and are often prescribed to people with severe cases of colitis.
Vedolizumab (Entyvio): This medication is prescribed to treat ulcerative colitis in people who do not respond to other treatments or cannot tolerate other medications.

- Other drugs
Additional medications may be needed to manage specific symptoms of ulcerative colitis. Your doctor may recommend one or more of the following:
Antidiarrheal drugs such as loperamide (Imodium A-D)
Housing
Antispasmodic drugs
Iron supplements
Intestinal colitis surgery
In more severe cases of intestinal colitis, surgical treatment is recommended. Surgical treatment of intestinal colitis includes the removal of the entire colon and rectum (proctocolectomy). Two types of proctocolectomy methods are used to treat ulcerative colitis:
Proctocolectomy with ileal-anal pouch anastomosis: removing the colon and rectum and creating an internal pouch where a permanent external ostomy is no longer needed.
Proctocolectomy with a terminal ileostomy: This procedure involves removing the colon, rectum, and anus and creating an external ostomy.
Diet for Ulcerative Colitis
Although a specific diet is not thought to play a role in developing ulcerative colitis, specific dietary changes can help control the disease. Paying attention to the following points may be helpful for you:
Eat small meals
Eating smaller meals daily instead of 3 main meals may help control your symptoms.
Drink plenty of fluids.
Dehydration is very likely if you have ulcerative colitis because you lose fluids through diarrhea. Water is the best source of hydration, and you should not use alcohol, caffeine, or carbonated drinks instead. These drinks can aggravate diarrhea and cause bloating.

Prevention of ulcerative colitis
Some foods can lead to intestinal inflammation and, as a result, colitis. Avoiding eating these foods can prevent ulcerative colitis. Some of the foods that should be avoided are:
alcohol
caffeine
Carbonated drinks
Dairy products (especially in people with lactose intolerance)
Beans, peas, and legumes
dry fruits
Different types of berries
Fruits with seeds or pulp
Foods containing sulfur or sulfate
Foods rich in fiber (including products containing bran)
Hot sauces
Spicy foods
Meat
Nuts and nut butter like pistachio butter
popcorn
Products containing sorbitol (sugar-free gum and candies)
Raw vegetables
Refined sugar
Grains

Conclusion
In ulcerative colitis, the inflammation starts from the rectum and may even spread to the colon. Ulcerative Colitis symptoms can be constant or come and go. Among the most acute symptoms of ulcerative colitis are diarrhea, weight loss, abdominal cramps, anemia, and blood or pus discharge from the intestines. There is no cure for ulcerative colitis; medications can only relieve intestinal inflammation.
Share in :
Explore more


Sitting A Long Time And Being Overweight- Drhealthandbeauty


3 Responses
My father had a digestive system problem. I don’t know its scientific name, but I think my stomachache is hereditary.
It can be, but I definitely suggest that you consult a specialist doctor.
Early diagnosis can prevent possible risks.
Your article helped me a lot, Thanks!